MUMBAI: Even as health crises in India grew, National Health Mission (NHM) funds unspent by states over five years to 2016 increased by 29%, according to a recent audit by the government’s auditor. The audit by the Comptroller and Auditor General (CAG) of India also reported delayed transfers and misallocation of these funds.

The NHM, launched in 2005, is India’s largest health programme aimed at providing universal access to healthcare. One of its primary missions is to improve maternal and child health and control communicable and non-communicable diseases.
Data show why it is critical that NHM funds be used optimally: India still accounts for 17% of global burden of maternal deaths, non-communicable diseases made for 61% of deaths in 2016, communicable diseases like leprosy and malaria are yet to be controlled and 55 million Indians slipped into poverty in 2011-12 because of health catastrophes they could not afford.
NHM also disburses funds to state health societies to help strengthen local health systems, institutions and capabilities. Rural health centres in India are short of human resources and infrastructure, as Indiaspend reported on January 30, 2018. Sub-centres were 20% short of human resources, 29% of them did not have regular water supply, 26% lacked electricity supply and 11% were not connected by all-weather roads.
India ranks lower than neighbouring Bangladesh and even sub-Saharan Sudan and Equatorial Guinea on healthcare access, we reported on May 23, 2018. And it spends 1.4% of its gross domestic product (GDP) on health, the least among BRICS nations.
In a two-part series, we look at the government auditor’s assessment of NHM’s functioning. In part one, we report on instances of financial mismanagement. The concluding part will detail the shortfalls in infrastructure and medical staff caused by this mismanagement.
The government has denied charges of financial irregularity. Funds were being released as soon as states fulfilled the requirements for their allocation, according to Manoj Jhalani, additional secretary and mission director, NHM.
“The diversion of NHM funds for non-NHM purposes/state government schemes is never supported by the ministry,” he said. “If any such instance comes to (our) notice, the same is recovered from the concerned state government, and states are directed to desist from such practice.”
Delayed transfers, misallocation and a growing balance
Our analysis of the CAG audit highlighted the following problems in the disbursement and usage of health funds:
- The amount unspent by state health societies went up from Rs 7,375 crore ($1.44 billion) in 2011-12 to Rs 9,509 crore ($1.43 billion) in 2015-16.
- State treasuries delayed the transfer of Rs 5,037 crore ($806 million) and Rs 4,016 crore ($ 606 million) released in 2014-15 and 2015-16 to state health societies. The transfer that is supposed to take 15 days took between 50 to 271 days.
- In six states — Andhra Pradesh, Gujarat, Jammu and Kashmir, Rajasthan, Telangana and Tripura — Rs 36 crore was diverted to other schemes, such as the Mukhyamantri Shubh Lakshmi Yojana (chief minister’s scheme for baby girls) and the Sukhibhava Scheme (assistance for institutional deliveries) in Telangana, and so on.
18 states spent only 32% of allocation which was already 36% short
In 18 states, against a requirement of Rs 133 crore, reflected in the 2013-16 state programme implementation plans, only 64% was allocated, we found. But states were not able to utilise even the allocated amount, with no more than 32% or Rs 43 crore spent.
“There are a number of reasons for unspent funds, ranging from the lack of human resources to complicated procedures for procurement in construction-related activities,” said Avani Kapur, fellow at the Centre for Policy Research and Director of the Accountability Initiative. “Another key factor is the uncertainty in the timing and amount of funds received under the scheme. There is often a mismatch in the what the state/district administration demands and what is actually approved and received.”
NHM is funded by both the central government and the states, with the centre providing 60%. The ministry of health and family welfare used to release funds directly to the state health societies till 2013-14. The money is now sent to state governments, which then move it to the societies.
The state-level societies in turn, disburse the funds to district health societies for further release to blocks. From here, the money goes to various implementing units such as community and primary health centres and sub-centres and village health sanitation nutrition committees.
NHM funds are released in five parts: NRHM Reproductive and Child Health (RCH) Flexipool, National Urban Health Mission (NUHM) Flexipool and Flexipool for Communicable Diseases and Non-communicable Diseases, including injury and trauma and infrastructure maintenance.
“One of the reasons for the creation of these (state health) societies was that the unspent money gets carried over to the next year unlike the state treasury which has to return unutilised funds at the end of the financial year,” said Kapur.
There are significant delays in the receipt of funds as CAG reported too, she said. “Given that states/districts have to prioritise routine activities such as salaries and Janani Suraksha Yojana payouts, there is an incentive to not spend money till the funds reach specifically (for certain projects),” she said. “Our research has thus shown that a lot of the softer expenses such as IEC (information, education, communication) or training often remained neglected.”
There are other problems with central sponsorship of schemes like NHM. Item-wise budgeting means that states do not have the flexibility to spend as per need, said Kapur. “I have heard the case of Himachal Pradesh where ASHAs (accredited social health activists) were not needed at one time but had to be hired because of NHM norms,” she said. “Under the new norms of the 14th finance commission, there is a provision wherein 25% of the funding is completely untied. (I) haven’t yet seen how states have operationalised this though.”
Unspent funds ranged from 40% to 76%, Meghalaya spent least
State health societies had spent only Rs 1,06,180 crore ($ 20.7 billion) of the Rs 1,10,930 crore ($ 17.1 billion) available during 2011-16. In some states the unspent balance ranged between 40% to 76% — for example, in 2015-16, in Meghalaya it was 76% and in UP, 52%.
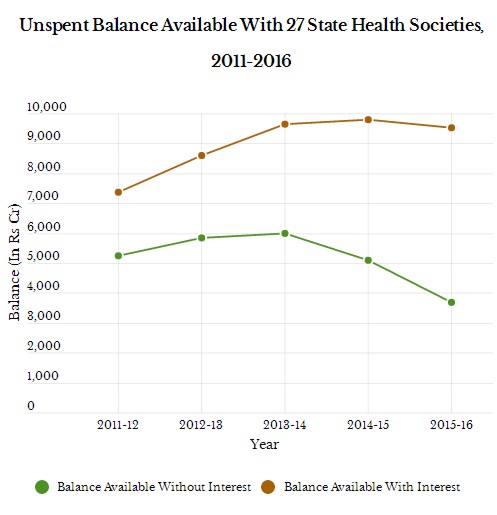
Source: Comptroller and Auditor General of India
The table above shows the unspent balance without interest and with interest (as mandated by the NRHM guidelines). In 2011-12, the unspent balance available with 27 state health societies without interest was Rs 5253 crore ($ 1.02 billion) which came down to Rs 3686 crore ($ 555 million) in 2015-16. However, over the same period, the unspent balance, including interest, with 27 states increased from Rs 7375 crore ($1.44 billion) to Rs 9509 crore($1.43 billion) .
Defaulting state are not being penalised, as procedure requires
States that do not spend the money given to them must be penalised, according to procedure laid out by the Union Cabinet and applicable from 2014-15.
State governments had to release the money to state health societies within 15 days of receiving it, and if they failed to do so state governments were liable to pay interest — 5.75% to 7.25%, depending on the going bank deposit rate.
The audit observed that Rs 49 crore released during 2014-15 and Rs 450 crore released during 2015-16 under Mission Flexipool and RCH Flexipool to state treasuries were not transferred to state health societies as of May 2016.
When asked to explain, the ministry told CAG that from time to time states had been asked to ensure timely release of funds to health societies. However, the CAG observed that the ministry had no answer when it was asked about action taken against defaulting states.
Operational guidelines for the funds also provide for money to be used for only specific targets. In six states (Andhra Pradesh, Gujarat, Jammu and Kashmir, Rajasthan, Telangana and Tripura), Rs 36 crore was diverted to other schemes as mentioned earlier. The ministry admitted to CAG that it had not acted properly in diverting NRHM funds for non-NRHM purposes.
For the period 2011-15, utilisation certificates (UCs) of Rs 4,283crore, under Mission Flexipool, were pending in 22 states/UTs. Under RCH Flexipool, UCs of Rs 3,175 crore were pending from 21 states/UTs as of May 2016.
‘Poor data management’
“Data management processes are under NHM are very poor, we have also found that data is often poorly maintained,” said Kapur who has authored the budget study on the NHM. “The inability to maintain data management systems has a consequence on planning for the next year as well as implementation. UCs need to show utilisation and the failure to submit it has implications for future rounds of fund release.”
Lack of staff and high vacancies mean that frontline functionaries have to produce and maintain most records without any clarity on how and when it will be used, Kapur said.
In its response to our questions, the ministry of health and family welfare has said that it has already put in place a slew of measures to deal with these problems: regulation of fresh funds, the use of the Public Financial Management System which provides a digital platform for fund management in real time, audit of state funds, training and review of state finance staff and the immediate transfer of funds between state health societies and state treasuries.
The central government is also advocating the use of single bank account in state operations so that in order to keep track of unspent funds, according to Jhalani.
(This is the first of a two-part series.)
Next: Upto 38% Shortfall In Medical Staff At Health Facilities Across India
(Salve is an analyst with IndiaSpend.)
Courtesy: India Spend