Why aren’t institutional deliveries resulting in fewer deaths during childbirth? Simply incentivizing institutional deliveries isn’t enough to push down MMR and infant mortality rate
Surujmuni Marandi, 24, had decided to deliver her baby at the Godda district hospital in north-eastern Jharkhand. Like many other women, she was drawn to the idea of free medical assistance, medicines, nutrition and postnatal care for poor, pregnant women promised by Janani Suraksha Yojana (JSY), the government programme aimed at reducing India’s high maternal mortality rate (MMR).
Marandi ticked all the boxes in the JSY profile of a woman who needs to be incentivised to deliver in a hospital: She was an adivasi, poor, had little access to health facilities, and would have gone for a traditional home-birth if it wasn’t for the scheme. Marandi should have had an easy time delivering her son at the hospital. But, as this documentary by activist media group Video Volunteers shows, she is denied everything that JSY promises.
Marandi, debilitated by labour pain, was made to wait six hours for a doctor who finally did not turn up for duty. She was asked to pay for medical attention and medicines and denied the nutrition and care that was her right. Denied basic facilities, even the use of a toilet, she finally delivered with the help of a nurse.
“We don’t know where the doctor is. You go, find out,” the nurse told Marandi’s mother when she asked for assistance.
Marandi’s story holds answers to India’s maternal mortality puzzle: Despite a rise in institutional deliveries, maternal mortality continues to be a worry for in India.
The number of institutional deliveries rose by 15% over the decade ending 2014, mostly aided by the JSY, according to this 2016 report by the think tank Brookings India, based on National Sample Survey Office (NSSO) data. Deliveries in government hospitals rose by 22%, fell by 8% in private hospitals and home-births dropped by 16%. But 167 women are still dying per 100,000 live births, as per latest government data. This is despite a 70% fall in MMR over a quarter of a century.
Why aren’t institutional deliveries resulting in fewer deaths during childbirth? Simply incentivizing institutional deliveries isn’t enough to push down MMR and infant mortality rate, wrote Ambrish Dongre, fellow at the Centre for Policy Research, in his 2014 analysis of the JSY. Physical and human infrastructure for maternal health and the quality of care too should improve, he said.
An IndiaSpend analysis of multiple reports and studies shows that Dongre’s analysis is right. The public health infrastructure, it appears, is simply unable to support the rising number of institutional deliveries that the government is encouraging. And this could possibly explain why India’s MMR is worse than Sri Lanka (30), Bhutan (148) and Cambodia (161) and the entire Arab world, as IndiaSpend reported in August 2016.
Painless, free care for pregnant women? Not quite
JSY is a 12-year-old government programme focused specially on 10 states with low rates of institutional delivery–Uttar Pradesh, Uttarakhand, Bihar, Jharkhand, Madhya Pradesh, Chhattisgarh, Assam, Rajasthan, Odisha, and Jammu and Kashmir–termed as low-performing states (LPS).
The other 19 states are clubbed together as high-performing states (HPS).
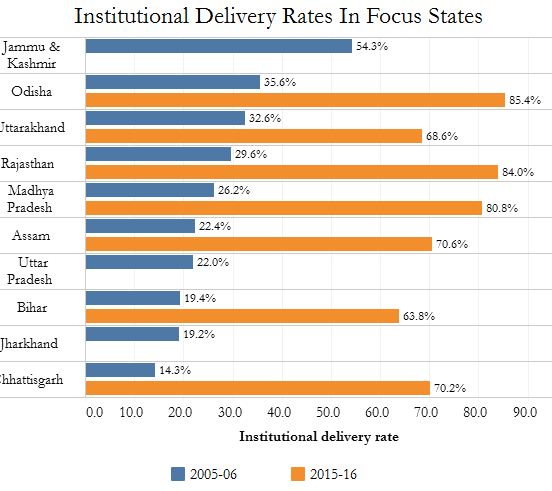
Source: National Family Health Survey 2005-06 and 2015-16
Under the programme, pregnant women in rural areas who live below the poverty line are to be given cash assistance–Rs 700 in HPS and Rs 1,400 in LPS–irrespective of the mother’s age and number of children, so that they opt for birth in a government or accredited private health facility.
In addition, it provides performance-based incentives to women health workers, ASHAs or Accredited Social Health Activists, to promote institutional deliveries.
In reality, the JSY has failed to cover the poorest women, according to this 2014 analysis of JSY data by researchers from Georgetown University. Some focus states report MMRs that match those of world’s poorest countries–Mauritania (320), Equatorial Guinea (290), Guyana (250), Djibouti (230) and Laos (220), IndiaSpend reported in September 2015.
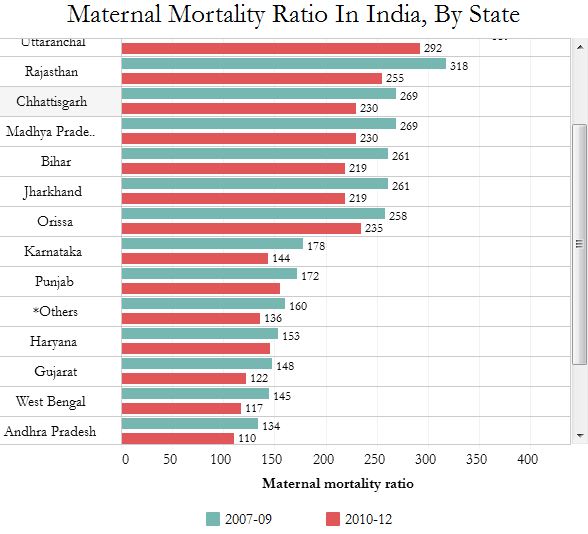
Source: Ministry of Health & Family Welfare
There is a lack of association between MMR and the rise in institutional births, according to this 2013 report, which analysed different government data for 284 districts across nine focus states. It is likely that women most vulnerable to maternal death are not getting the JSY benefits, the report said.
Marandi’s story is repeated in hospitals across India, like this one in Bankeda village in western Odisha’s Subarnapur district. Families of patients are forced to hire private vehicles, pay for check-up and delivery at government health facilities. They do not receive cash incentives–Rs 1,400 under JSY and Rs 5,000 under the state’s Mamata Yojana. “Why should we go to state-run health facilities?” the women ask.
As in Marandi’s case, 60% of women in Uttar Pradesh said they had to pay for certain public maternal health services, according to an assessment of JSY conducted by United Nations Population Fund in Bihar, MP, Odisha, Rajasthan and UP in 2012, IndiaSpend reported in September 2015.
Prime Minister Narendra Modi announced that Rs 6,000 would be transferred directly to the bank accounts of pregnant women who undergo institutional delivery/and vaccinate their children. But as FactChecker found, the option of giving Rs 6,000 to pregnant women already existed in the National Food Security Act (NFSA), 2013–it just had not been implemented by the government.
Not enough doctors, not even toilets at health facilities
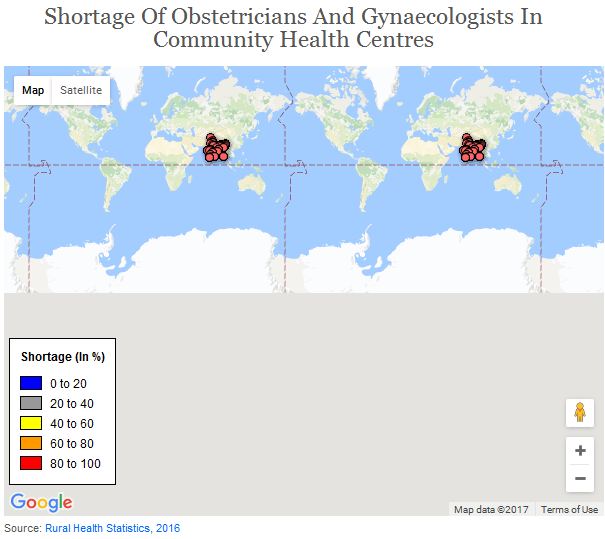
There is a 77% shortage of obstetricians and gynaecologists in Community Health Centres (CHCs) nationwide, according to the Rural Health Statistics 2016 released by the ministry of health and family welfare. And 15 states and union territories have more than 90% shortage of obstetricians, gynaecologists in CHCs.
The CHCs constitute the secondary level of health care. These provide specialist care to patients referred from Primary Health Centres (PHCs), four of which feed into each CHC, serving roughly 80,000 people in tribal, hill or desert areas and 120,000 on the plains.
Nearly 62% of government hospitals–which include CHCs, district hospitals and sub-district hospitals–don’t have a gynaecologist on staff and an estimated 22% of sub-centres are short of auxiliary nurse midwives (ANMs), IndiaSpend reported in September 2016. Additionally, in 30% of India’s districts, sub-centres with ANMs serve double the patients they are meant to.
Sanitation facilities at public health centres where women deliver are inadequate as well. In the video, Marandi can be seen struggling to find a toilet after she is given laxatives before childbirth. In one instance, she simply squats outdoors in public to ease herself.
This is not unique to Godda. There are no toilets in half the postnatal wards of PHCs, as is the case with 60% of larger CHCs in MP, according to a study by WaterAid India in 343 healthcare institutions across six states and reported by IndiaSpend in July 2016. Open defecation was allowed within 38% and open urination in 60% of health facilities in Odisha’s Ganjam district, according to the report.
This should not come as a surprise: Of the 4,000-odd multi-crore infrastructure projects in the country, only nine (0.21%), with a total investment of Rs 938 crore, are in the health sector, IndiaSpend reported in December 2015.
There is no guarantee of quality care
“The government encouragement of institutional deliveries is based on the idea that poor people choose to deliver at home either out of ignorance or an inability to make the right decisions or due to cultural norms and the exercise of (male) power,” argued Jishnu Das, lead economist, World Bank in a 2014 blog. “But an alternate starting point is that people were not using institutions to begin with precisely because quality was low, and that increasing quality would also bring more people in.”
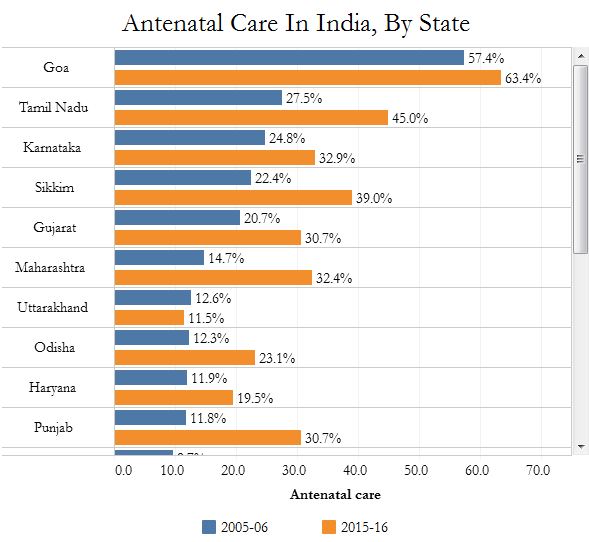
The quality of antenatal care is vital to reduce the risk of stillbirths and pregnancy complications, and the absence of it explains why more women enrolling for hospital deliveries does not translate to fewer maternal deaths.
In Odisha, only 23% of women reported receiving full antenatal care, the highest among focus states, according to National Family Health Survey data for 2015-16 (NFHS-4). The figure in Tamil Nadu, which is considered one of the best states to be a mother, was 45%. Only 3.3% of women in Bihar reported receiving full antenatal care, a decline from 4.2% in 2005-06.
Full antenatal care equates to at least four antenatal visits by health workers, at least one tetanus toxoid injection and iron folic acid tablets or syrup taken for 100 or more days.
Source: National Family Health Survey 2005-06 and 2015-16.
Most obstetric complications could be prevented or managed if women had access to a skilled birth attendant–doctor, nurse, midwife–during childbirth, according to the World Health Organization.
The probability of maternal death among Indian women decreased with increasing skilled attendant coverage, among both women who were and were not admitted to a health-facility, according to this 2014 analysis of different government data.
(This story is the result of a collaboration between Video Volunteers, a global initiative that provides disadvantaged communities with story and data-gathering skills, and IndiaSpend. Saha is an MA Gender & Development student at Institute of Development Studies, University of Sussex.)
You can see the full playlist of Video Volunteers’ videos–revealing gaps in maternal-health services–here.